Dysplasia: what do we mean?
G. E. MacLellan MBBS. FRCS. CCST. Orthopedics.
Is Dysplasia a diagnosis?
The short answer is NO. Dysplasia is a word taken from ancient Greek and simply means disordered or faulty development. It is used to describe abnormalities of bones, kidneys, blood vessels and every other anatomical structure in the body, both human and canine.
A diagnosis is made by taking a history of symptoms, past and present, conducting a clinical examination and then confirmation by special investigations such as blood tests, X-rays, scans etc. Your Vet can only request the appropriate special investigations after taking the history and carrying out the clinical examination. Your Vet does not need to be a Specialist to try to make a diagnosis but may recommend Specialist advice if there is more than one possible diagnosis. “Differential” diagnosis means sorting out the different causes of an abnormality of anatomy or function. Pathology is the study of processes that have gone wrong. It is usually broken down into two broad groups, congenital (meaning born with it) and acquired.
What we have learned from human medicine that may be helpfully applied to dogs.
“Congenital” may indicate a genetic disorder but, just as importantly, might also be the consequence of a hostile intra-uterine event or environment. Many genetic disorders do not survive to birth and in dogs may resorb or be still-born.
In human medicine we are familiar with the severe effects of toxins in pregnancy ranging from smoking (including passive), alcohol and drugs such as Thalidomide. Maternal malnutrition causes low infant body weight, or a folic acid deficiency may cause spina bifida but there are numerous other acquired nutritional problems. The intra-uterine environment such as too little amniotic fluid or an abnormality of uterine shape, can cause joint deformities in babies ranging from club foot to congenital hip dislocation, but prompt treatment after being born can sometimes completely correct these deformities and they are not a contra-indication to then having children. There are even infections that can be acquired during birth. If the birth canal is infected it can result in “congenital” cataract, which is not always genetic but often an acquired infection. There are countless other examples of congenital disorders in children that are not genetic.
Acquired pathology after birth arises from trauma, infections, toxins, radiation, malnutrition including vitamin deficiencies, tumours and many other factors, but these must be differentiated from genetic faults. Some genetic diseases arise during growth or in adult life such as Huntingdon’s Disease or Chronic myeloid Leukaemia due to the Philadelphia Chromosome.
Epilepsy is a good example of a condition that has numerous causes. Although a family history is common, so is head trauma, whether at birth or later in life. Brain infections by viruses or bacteria and tumours, both benign and malignant, are frequent causes of epilepsy in humans and dogs, so it is essential not simply to blame genetics for all fits.
Different human races have different diseases that may influence skeletal development. Thus Gaucher’s disease in Jewish populations or Sickle Cell Disease in Africans both may give rise to skeletal problems but through totally different pathological processes. In some societies there are moves to genetically screen parents-to-be in an attempt to avoid these problems, as breeding outside a known community may conceal these genetic traits that may emerge two or more generations later.
In dogs it is believed by some, that cross breeds have fewer genetic problems than Pedigree and Line-bred dogs but this is far from the truth. For example, there is no evidence that cross breeds have a lower incidence of Hip Dysplasia than line-bred dogs (Prevalence of inherited disorders among mixed-breed and purebred dogs: 27,254 cases 1995-2010. Bellumori T.P. et al Journal of the American Veterinary Medical Association June 1, 2013, Vol 242 No 11, Pages 1549-1555). Cross-breeders can seldom produce three generation health information for the puppy buyer and most carry out no health checks on the sire and dam, let alone on the puppies.
It is therefore reasonable and responsible to apply the same rules of evidence based medicine in dogs as in humans.
Hip joint development.
Since the discovery of clinical X-Rays by Roentgen in 1895, they have been used to diagnose a wide range of skeletal disorders in humans and animals. However, before the second world war their use in Veterinary practice was not routine or widespread, as reported by Russel Beamer in 1939 (The significance of X-Ray in Veterinary medicine. Iowa State University Veterinarian: Vol1; iss 3, Article 7).
As X-Rays became more widely used, the diagnosis of hip ‘dysplasia’ was made more commonly and naturally, was diagnosed more frequently in the commonest breeds, some of which then became associated with an increased risk of developing the problem. During the 1960s, researchers in Sweden (On the Etiology and Pathogenesis of hip dysplasia: a comparative review. Henricson B., Norberg I., Olsson S-E. Journal of Small Animal Practice Vol7,1966:673-688 ) tried to establish what was going on in dogs and found marked similarity with human hip dysplasia, then known as Congenital Dysplasia of the Hip (CDH). Human and Veterinary Researchers put their heads together and concluded that there were such marked similarities, that they stated that “Hip dysplasia can be taken as a good example of a disease in which comparative studies can contribute to an increased knowledge of the aetiology, pathogenesis and treatment”.
The Swedish group believed that environmental factors were probably responsible for about 50% of all cases of hip dysplasia and that “the cause of laxity is unknown and future research has to be focused on this problem”. In the subsequent years the canine living environment has fluctuated along with changes in human habitation. Day to day canine activities and nutrition have also changed out of all recognition compared with the 1960s. Despite this knowledge has there been a change in how we have come to think of hip dysplasia in dogs? Not yet, it seems.
In humans, we saw the introduction of CT scanning to give us three dimensional understanding of X-Ray imaging in the 1970s but this was not widely available to Veterinarians for many years. Even today the decision to CT scan a dog must be balanced against the risk of the anaesthetic that is always needed to keep the dog still during the procedure, as well as risks associated with irradiation of the gonads in dogs being considered for breeding. Thus, comparative studies were late in arriving for dogs. In the UK most hospitals did not have access to CT scanning until the late 1980s when various local charities were set up by their hospitals to buy a scanner. With the advent of Magnetic Resonance Imaging (MRI) in the 1990s human imaging diagnostic machines were also bought after local charity fundraising for the NHS.
The Veterinary world had much less access to such scanning technology because funding was so scarce . In many cases the equipment used in ‘human’ hospitals that was being replaced 10 or more years later was sold to Veterinary hospitals and so became more available for dogs.
The same challenges arose with the introduction of Isotope scanning for children with hip problems. The period of rapid advance was again the 1970s. The excitement of discovering that changes in a child’s hip due to Perthes disease could be seen on isotope scanning, weeks before there were any X-Ray changes broke new ground in 1976. This brought together the relationship between the X-Ray image and the stages of the pathological disease progress that allowed new approaches to treatment. Big decisions about the benefits of surgery versus conservative management could be made on both anatomical and pathological evidence for the first time.
In 1982 the use of ultrasound imaging of the human infant hip in the first six weeks of life was first validated. At this age X-Rays cannot show the femoral head (ball) as it is entirely made up of cartilage, as is most of the socket (acetabulum) so X-ray diagnosis was severely limited.
Clinical examination of infants using Barlow or Ortolani tests were taught to all Paediatricians and Orthopaedic surgeons. The advent of reliable non-invasive, non-sedated ultrasound imaging not only allowed accurate diagnosis, but could also guide management of the condition as scans were repeated without hazard to the baby.
In dogs a peer reviewed publication from Brazil in 19 puppies revealed no cases of hip dysplasia. Importantly, it also demonstrated that reliable images of the developing canine hip could be produced (Ultrasonic and Radiographic study of laxity in hip joints of young dogs. Rocha B.D., Torres R.C.S. Brazilian Journal of Veterinary and Animal Science. 2007; 59:90-96.
The research in Brazil does not appear to have continued and little more was published, nor after a study from Germany (15) in 2010 of 566 pups scanned with no cases of hip dysplasia found. There appears to have been no further progress made. Nevertheless, evidence was building that congenital hip dysplasia at birth is uncommon in the breeds studied.
In 2016 the Pupscan Research Project in The United Kingdom and Ireland started scanning puppy hips using exactly the same methodology and personal experience of human infant orthopaedic practice since 1985.
Because of the great diversity of breeds, their functions and development, an early decision was made to scan at least 2,500 puppies in as many breeds as possible. This target was achieved by January 2020 in over 70 breeds with the youngest scan in a nine day old Shiva Inu and the oldest, a 16 week German Shepherd.
Ultrasound Doberman hips, four weeks
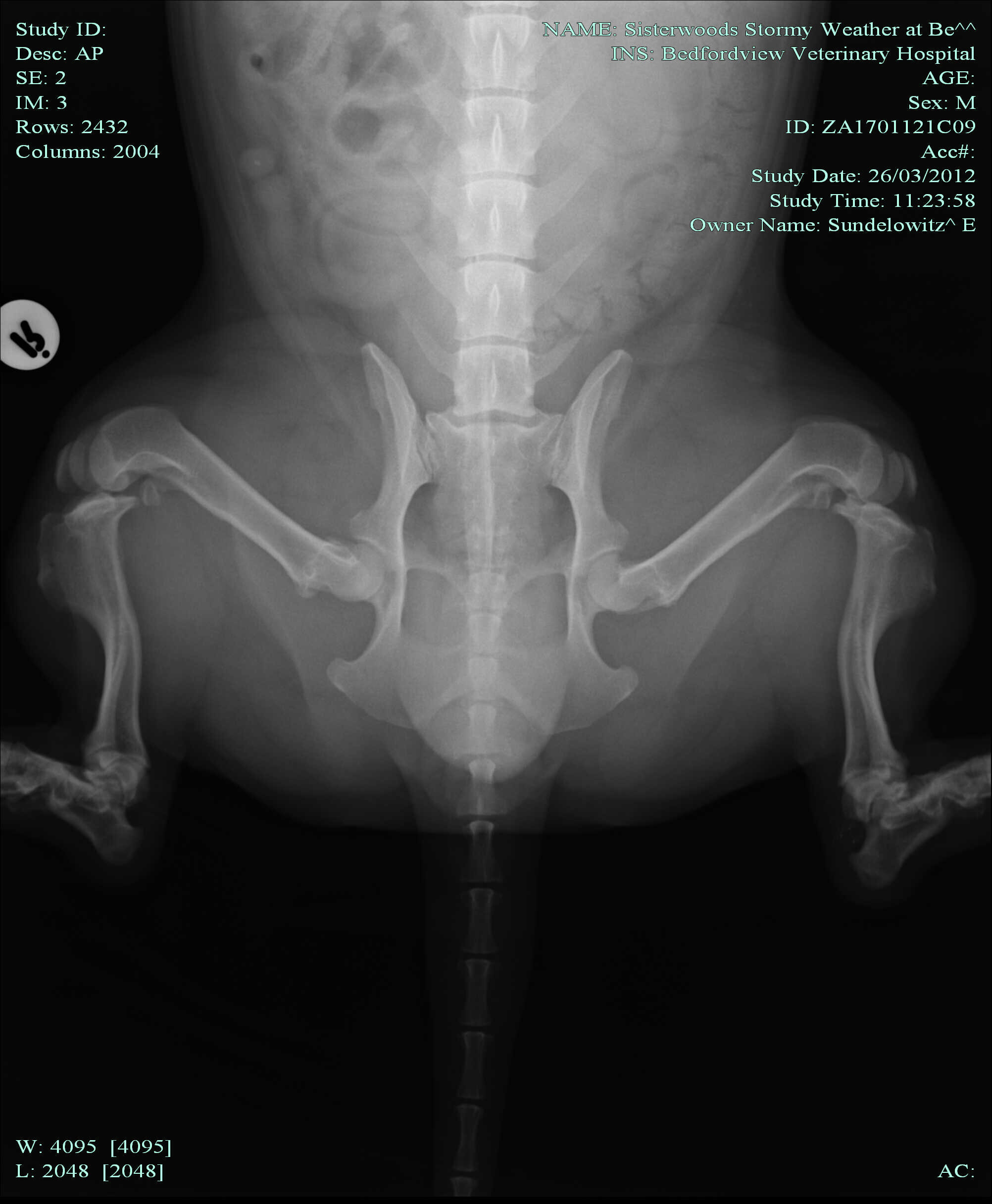
Because of the perceived increased susceptibility of larger breeds to hip dysplasia they received particular attention. However hip dysplasia in small and Toy breeds is well known, as in this image of a Pomeranian.
Severe bi-lateral hip dysplasia in a Pomeranian.
The Pupscan Project found its first dysplastic hip in a male Retriever, the smallest of the litter. All of the five other puppies had normal hips. By chance the breeder was a Veterinary Surgeon so planning future care and observation was not a difficulty. The puppy was separated from his litter mates but otherwise given normal care. Three weeks later a follow-up ultrasound scan showed a developing acetabulum (socket) and the femoral head seemed to be developing normally though ossification was a little behind the healthy hip. This corresponds with human experience. The puppy grew well, putting on weight as fast as his litter mates. He matured into a fine adult with no disability and was a success in the show ring.
Since then there have been three more dysplastic hips found at about six to eight weeks of age. All have been managed the same way and all developed a good acetabulum. All were unilateral.
So after 5 years of Pup-scanning, together with the previously reported hip ultrasound scans what have we learned?
Congenital hip dysplasia exists in dogs as well as humans but it is RARE. Under eight weeks of age the incidence is less than 1 in 1000 hips from 70 breeds scanned to date. Congenital Canine hip dysplasia in all breeds is much rarer than in humans, but from this early experience a functional approach to management seems to be appropriate.
In human infants we use a dynamic hip brace (such as the Pavlik or Wheaton harness) to support the ball in the socket while the hip grows. If the baby grows quickly, so does the socket. The same appears to apply to dogs. The two species appear to be comparable.
Was the cause predominantly genetic in the puppy? It seems unlikely. It is more probable that the intra-uterine environment was at fault as all were from an otherwise healthy litter and only one hip was involved. If the cause was predominantly genetic, both hips should have been involved to some degree, as in humans. In terms of genetics it makes no sense to only involve one joint.
The Pupscan Project has identified two hips that showed evidence of injury to the growing acetabulum before 10 weeks of age.
The first was a giant breed puppy having a routine scan and shown to be normal only three days before leaving for its new home. A child left the puppy gate open and the owner heard a yelp from the kitchen. The puppy had gone to play with the other dog in the household and fell on the slippery floor. The Pupscan team were able to visit the puppy at its new home and re-scan the hip only three days after the previous scan. There was an effusion (fluid) in one hip joint and evidence of an injury to the rim of the acetabulum where the bone and cartilage met. The findings were demonstrated to the owner who agreed to rest the pup in a cage for 10 days in the hope that the injury would heal without displacement. The puppy settled well and grew with no disability. No skeletal maturity X-rays are available.
The second was an energetic pastoral pup with an acetabular rim injury found on the planned and scheduled six week scan. An unstable fracture line containing joint fluid was seen on the scan at the bone- cartilage junction of the acetabulum. On extending the hip backwards the femoral head rose in the socket, causing the injured rim to tilt upwards. The same management was followed. The scan three weeks later showed the fluid to have disappeared from the fracture line and the rim had become stable. Healing callus was seen beneath the periosteum. Three weeks later the hip was clinically normal and fully stable on the ultrasound scan. This is the only dog with this injury we have seen to have had an X-ray at skeletal maturity and this showed a normal hip joint.
Both these cases are examples of one-sided hip joint laxity following trauma to the rim of the socket, one of which has been confirmed by skeletal maturity X-Ray to have healed with no joint abnormality. The other has never been X-rayed so the outcome is unknown. No surgery or brace treatment was undertaken but both were strictly prevented from repeated trauma immediately on diagnosis.
Both these cases confirm the importance of the living environment, as emphasised 50 years ago by the Swedish researchers (4). The first was energetic play on a slippery floor with a larger mature dog and the second play with boisterous litter mates on a soft surface. Neither case had a genetic component and neither had a family history of hip dysplasia.
Other animal research shows how the acetabular growth can be influenced by trauma. A study on rabbits in which the growing cartilage in the floor of the acetabulum was surgically damaged resulted in poor socket growth (Premature closure of the tri-radiate cartilage. A case report and Animal Experiment. Hallel T., Salvati E.A. Clinical Orthopaedics and Related Research 1977 May;(124):278-281).
A remarkable experiment was reported in 1999 (5) on six week old puppies in which the acetabular rim (labrum) was stitched back to the side wall of the socket and produced typical features of acetabular dysplasia. Interestingly they also noted that the joint capsule stretched post-operatively as the acetabular rim failed to grow, the joint progressively began to subluxate and the articular cartilage started to degenerate. (Acetabular dysplasia and Osteoarthritis Developed by an Eversion of the Acetabular Labrum. Kim Y-H Clinical Orthopaedics and Related Research 1987 Feb; No 215 pp289-295).
Evidence from human research again shows the importance of the acetabular labrum. In 1979 a review of total hip replacements showed that in a large number of cases of simple osteoarthritis of the hip, the labrum was torn and turned in to the joint (Intra-articular acetabular labrum: a possible aetiological factor in certain cases of osteoarthritis of the Hip. Harris W.H., Bourne R.G, Oh I. Journal of Bone and Joint Surgery 1979;61:510-514). The area of total loss of articular cartilage from the femoral head was always where it had been in contact with the displaced and torn labrum. A subsequent study showed that labral lesions were extremely common, present in 93% of specimens (McCarthy et al. 2003.Acetabular and Labral Pathology. Early Hip Disorders pp 113-133).
In humans the labrum is involved with circulation of joint fluid during load-bearing activity, working a bit like a one-way valve (A Post-mortem study of the hip joint. Byers P.D., Contepomi C.A., Farkas T.A.. Annals of Rheumatic Diseases 1970 Vol 29; pp 15-31). If the labrum is torn, this function is lost (The torn Acetabular Labrum. Dorrell J.H., Catterall A. J Bone and Joint Surgery 68Br. pp400-403 1986.
The human labrum is not quite the same as in the dog. In humans it almost completely encircles the joint, being absent only at the bottom of the socket where the round ligament passes to the femoral head through the acetabular notch. In dogs our dissections have revealed that towards the head and the tail the fibro-cartilaginous labrum is well formed but in the dorsal area it appears to be small or absent. We hope that further studies by Veterinary anatomists will be able to study more breeds in the next few years to establish what variants are normal and where the joints are arthritic, if it is the result of a labral injury.
There are two sides to every joint!
Turning to the femoral side of the joint there is even more to learn! In humans there are two common and treatable problems that arise during growth.
A slip of the upper femoral epiphysis (SUFE) is common in adolescents, especially those doing a lot of contact sports (The Aetiology of Primary Osteoarthritis of the Hip. Murray R.O. MBE. British Journal of Radiology 1964 Vol 36. Iss455). This means that where the growing neck joins the spherical ball, an injury can cause the ball to displace. It may tilt a few degrees and heal with little or no ill effects in the long term but in humans a slip of more than 30 degrees is often followed by osteo-arthritis later in life.
Ventro-dorsal
Frog Lateral
Corgi with left slipped upper femoral epiphys. Note displacement of left femoral head compared with right. Not visable on the ventro-dorsal.
The mechanism by which the arthritis develops is now known to be an impingement of the resultant bump (the ‘cam”), on the junction between the femoral head and neck and the “pincer” of the rim of the acetabulum and our friend the labrum causing it to split or tear. It loses its function as a seal, makes the joint surface smaller and causes over-load on the cartilage surface.
In the human, adolescent SUFE is frequently mis-diagnosed as a “groin strain” and not properly diagnosed or treated, but if diagnosed early big slips can sometimes be replaced to a near normal position and then fixed with pins or screws so that further slippage does not occur during growth. Exactly the same procedure can be carried out in dogs if the diagnosis is made in time, probably within 24 hours.
Pinned left slipped upper femoral epiphysis
Once again we are looking at a form of hip dysplasia resulting from an injury during growth that occurs in both humans and dogs.
But is there a genetic contribution in dogs?
It was believed that two genes, COL2A1 and VDR could be responsible for some cases of dysplasia but these were excluded in 2008 (Clinical Orthopaedics and Related Research Vol 466(4):878-883). We know that in humans SUFE is correlated with periods of rapid growth in height or weight. There are rare human genetic disorders that could be a factor such as Prader-Willi Syndrome and recent canine research (Confirmation that a deletion in the POMC gene is associated with body weight of Labrador Retriever dogs. Mankowska M., Krzeminska P. et al Res Vet Sci 2017 Jun;112:116-118), has indicated a genetic pre-disposition to obesity which may prove to be more common in some breeds than others. Should we perhaps screen for this in selection of dam or sire for breeding?
Legg-Calve-Perthes disease and its avascular necrosis relations cause disruption to the blood supply or venous drainage to the head of the femur.
There may be many potential causes in dogs varying from the anatomy of the blood supply of the femoral head (arteries and veins) to the viscosity of the blood flowing in those vessels. The anatomy is doubtless genetic in origin but not every dog with anatomic variants will get Perthes. Without large dissection studies in different breeds we will not know the frequency or importance of the anatomic variations.
It is well known that an increase of fluid pressure in the hip joint results in Perthes disease (The experimental induction of sub-clinical Perthes disease in the puppy following arthrotomy and intracapsular tamponade. Singleton W.B., Jones E.L. Journal of Comparative Pathology. 89(1):57-71). The reasons for an increase of fluid pressure during normal canine activity is often not known, but it is very unlikely to be genetic and various traumatic episodes can often be recalled by the owner.
In children a virus has sometimes been identified in small research studies. Bacterial joint infections are much more severe and justify urgent investigation and treatment to prevent serious joint damage; these are always treated urgently.
Abnormal clotting in blood has been identified in some (but not all) children with Perthes, such as sickle cell disease and Factor 5 Leiden. The human genetic inheritance is well known but it has not yet been studied in dogs so this potential genetic cause in dogs is not yet known. Other blood clotting factors have been analysed in dogs without a helpful result (Analysis of blood clotting factor activities in canine Legg-Calve-Perthes disease. Brenig B., Leeg T., Jansen S., Kopp T. J Vet Intern Med Nov-Dec 1999; 13(6):570-573).
Episodes of transient lameness in a puppy are seldom investigated as X-Rays, CT and MRI scans need an anaesthetic which makes them risky as well as costly. Veterinary practitioners skilled in the use of diagnostic musculo-skeletal ultrasound can easily and safely identify excess fluid in the hip and advise treatment accordingly, potentially improving outcomes. With modern ultrasound scanners it is possible to tell the difference between blood and clear fluid in the joint, a great advantage over X-Rays and CT scans.
In children with Perthes disease we know that if load is taken off the hip while the femoral head is soft, the socket works like a jelly mould and the head will repair itself, often leading to an excellent hip for life.
The often used X-ray description of the femoral head as “fragmented” is not correct. The patchy appearance is of areas of soft bone with the calcium removed in preparation for repair; it is an essential part of the natural healing process. Sometimes there is a separate fracture fragment but this is uncommon.
If load is removed from the Perthes-afflicted hip joint while healing is allowed to progress, the femoral head may grow to be almost normal without any need for surgery. In children this takes a lot of support from the family as it can take many months, and sometimes as long as a year, for the femoral head to heal, but in the puppy only a few weeks are likely to be needed.
The principle of full containment of the femoral head in the acetabulum to stimulate development of both the depth and diameter of the hip socket is critical from early foetal life until skeletal growth is complete, always remembering that different breeds mature at different rates, just as in humans. (Bone age in children of Diverse Ethnicity. Ontell F.K. et al. American Journal of Roentgenology 1996; 167: 1395-1398)
In dogs it is a simple matter for them to get around on three legs while the damaged hip heals, so early ultrasound diagnosis could be the key to preventing early onset osteo-arthritis. Supportive hip braces for dogs are widely available to Veterinarians and many stock them in the clinic to start treatment promptly.
So what should BREEDERS mean by “hip dysplasia” in dogs? It is clearly not one disease but many, likewise Elbow “dysplasia” in which almost all the same differential diagnoses apply.
The essential first step is to abandon the generally used term “Dysplasia” if considering genetic inheritance. It means absolutely nothing in considering suitability for breeding without a DIAGNOSIS.
If it is on the socket side from birth it is acetabular dysplasia. That may be caused by the intra-uterine environment, such as an amniotic fluid leak or the dam may have had an infection at a critical stage of the pregnancy. Either sire or dam may have ingested a toxin leading to chromosomal damage or even been exposed to excessive radiation to the ovaries or testes, both environmental problems as opposed to genetic inheritance from the parents but some could be passed on to the next generation. Therefore MAKE THE DIAGNOSIS.
If acquired after birth it may be due to trauma, infection, malnutrition etc. and these questions must be asked and answered BEFORE blaming genetics.
On the femoral head side there are all the causes of a slipped upper femoral epiphysis as well as the effects of blood flow damage to the femoral head resulting in avascular necrosis. Very rarely a genetic cause may be identified.
It is vital to understand that all canine hip dysplasia is NOT genetic. From X-Rays sent to The Pupscan Project from all over the world we have seen examples of all the conditions described above.
It is also important to understand that IF genes are involved, they may be ones that determine personality and risk-taking in the puppy as well as ones determining anatomy, chemical processes or obesity (35).
The Pupscan Project has established after more than 5000 hip scans from entire litters (without pre-selection) in over 70 breeds of dog that puppies are very rarely born with dysplastic hips. The true incidence so far is less than one hip in a thousand.
Every breeder and Veterinarian must now satisfy themselves that environment, nutrition and injury have all been excluded as causes of joint development problems BEFORE blaming genetics. There are rare genetic disorders in humans that emerge during adolescence, but we will only be able to identify these in dogs if the puppy has been scanned in the first two months of life while still under the care of the breeder.
If puppy hips are scanned and proved to be normal before leaving the breeder it cannot later be alleged that the breeder sold a dog with dysplastic hips. This is a genuine health test on the puppy, independent of any investigation of the sire and dam.
Every scanned puppy gets its own certificate incorporating the microchip number for individual identification. This allows their information to be verified years later if a problem arises that needs to be explained. Over the years the project has been running several such cases have been referred for review and diagnosis. Puppies that have been scanned by the Project will only have a Certificate if all the necessary documentation for identification has been submitted. Certificates are not issued if the puppy is not fully and correctly identified, including the microchip number.
Are hip X-Rays still helpful?
Yes – very much so provided the images are designed to give a diagnosis.
It is particularly important not to subject the joint to traction in any direction. The rim of the socket may not complete its growth until six months or more after the thigh bone has stopped growing. Any amount of longitudinal traction on an immature socket could result in rim and labrum damage. Because of the anatomy of the ligaments in the joint and capsule of the hip either longitudinal traction, forced extension or lateral leverage may cause a tear to the capsule or the labrum. Should such an injury to the immature socket occur, it is very likely to cause osteoarthritis later in life if it does not heal correctly.
If labrum or capsule injuries heal with weak scar tissue it will be described on X-Ray under traction as “laxity”. Films with traction or leverage applied, as for “scoring”, have usually interpreted laxity as a genetic fault as opposed to the consequence of an earlier injury. Lameness following scoring is widely reported and therefore the injury might possibly sometimes be caused by the procedure itself.
The American Orthopaedic Foundation for Animals scoring system does not include traction or leverage of any sort. Furthermore, they do not accept images for scoring taken earlier than two years of age and are therefore unlikely to cause any labrum injury. The OFA recommends gonadal radiation shielding for male dogs and avoid spurious laxity in females by not imaging 3-4 weeks before or after a season (Orthopaedic Foundation for Animals Web Site 2021). Full identification of the dog on the image submitted is a requirement, including left and right side labels together with the Registration Certificate if available. The OFA also provide a Consultation service. Unfortunately some other schemes are less strict.
The best views for diagnosis are taken with the dog lying on its front, one with the hind legs parallel and fully extended (with no force applied) and the other in the 90 degree ‘frog’ lateral position. This allows the upper femur to be imaged with two views at 90 degrees to each other and reveal otherwise hidden problems such as slipped upper femoral epiphysis or Perthes disease involving part, but not all of the femoral head.
Further down the bones it is usually possible to get an indication of the bone quality by comparing the thickness of the cortex with the medulla. If the cortex is thin and the medulla wide, it might suggest nutritional deficiency and the possibility of weaker bones that are more prone to fracture. Clinical examination revealing generalised ligament laxity due to genetically inherited Ehlers Danlos Syndrome is also often associated with osteoporosis.
X-rays may also reveal very rare genetic diseases that damage bone quality. This is especially valuable when evaluating cross-breeds when the whole breeding history of the last few generations is usually unknown. Breeding from “Cross Breeds” is a risky business for the offspring compared with pedigree dogs in which responsible breeders have done their very best to prevent inherited diseases.
Chondrodysplasia is a major influence in short breeds and is clearly visible on X-rays; some chondrodysplastic dogs have temperament issues that are well understood by those familiar with the breeds, but such traits bred in to larger dogs could give rise to behaviours that are unwelcome or, with small children, dangerous; X-Rays may give a clue.
There are several genetic disorders that can be detected on standard X-rays that may indicate bone quality or kidney function problems that would be a strong contra-indication to breeding.
It is essential that the image quality is designed for diagnosing rather than simply getting a picture for phenotypic assessment. Images obtained using physical forces such as traction or leverage are of little or no value in making a diagnosis, other than to indicate an earlier injury that has healed with stretched scar tissue. Most of us are familiar with stretch marks and surgical scars in humans that heal wider than when first closed but this is not an indication of a genetic disease; It is simply a manifestation of the healing of any scar, be it in the skin, joint capsule or any other tissue and varies between individuals. Excessively dense scars are also a problem for joints which may be stiffened or contracted but again is part of the healing process and not an inherited joint disease.
Hip, knee or elbow joint laxity is far more likely to be due to an injury than any genetic problem, especially when the two sides are different. A further confusing factor is the sedation and relaxation of the dog used to take the X-rays. A study on hip scoring showed that scores increased when the standard anaesthetic agents used for the procedure were changed and resulted in an average increase of scores of almost 30% (38).
It is also essential to know the distraction force used to pull on the joint to decide if symmetrical laxity is of any significance. For example traction of 5 kg on a hip of a 10 kg dog is much more force than on a 60 kg dog and could be expected to produce an impression of much more laxity. Manual traction is even more difficult to assess, so all assessments of “laxity” on X-Rays must be considered very carefully if trying to make a diagnosis of pathological laxity.
In day-to day life the hip joint remains stable through muscle tone combined with joint congruity and suction maintained by the labrum seal (39); the ligaments are used very little. Even very dysplastic hips can function perfectly well for many years with regular moderate exercise, sometimes in suitable breeds supplemented with swimming if available. X-ray under traction is of little relevance to real life day-to-day activities.
This is not to say there is no association between joint laxity and osteoarthritis: in the knee joint of humans it is very well understood following trauma and sometimes Ehlers Danlos Syndrome(EHD) but the knee is not a fundamentally highly stable joint like the “ball and socket” of the hip. Even in Ehlers-Danlos the hips do not usually develop arthritis, let alone non-EHD Generalised Ligamentous Laxity. If that were the case every gymnast and dancer would suffer from multiple joint osteoarthritis later in life and they certainly do not!
X-rays of hips under anaesthetic using different pain relieving and joint relaxing drugs with undefined amounts of traction or leverage cannot be used for a meaningful diagnosis. Likewise elbows X-rayed from the side only are little help; If you need a diagnosis your vet will always take at least two views (A-P and Lateral) and sometimes also an oblique view to show the coronoid process clearly.
If you have a report that a hip joint is lax (perhaps as part of a high “score”) check the laxity of the skin and mobility of your dog’s knee and elbow joints; if they are normal you can be reassured that there is no genetically inherited disorder of collagen and that the hip laxity is most probably due to past trauma. It should not be a contra-indication to breeding on that assessment alone.
Beware a high laxity score on one side and a low score on the other. Genetic conditions will affect both sides equally. Using a combined score to make decisions on breeding is therefore a mistake.
Unilateral laxity
Genetic Testing.
Have any genes been identified as responsible for canine hip dysplasia?
Not yet. Several research groups have tried without success. Possibly a factor has been that genetic samples were taken from dogs with high hip scores but without an associated diagnosis for the high score. Since most dog owners do not score their dogs unless considering breeding from them (and even that is not universal), the studies are entirely pre-selected and of no statistical value.
Might any genes be identified?
Possibly. A good starting point would be to submit samples from dogs with a diagnosed disorder of hip development where factors such as environment, nutrition, trauma etc have been excluded.
When we get to a situation where thousands of litters of puppies world-wide are screened by ultrasound scanning under eight weeks of age, we will eventually find more dogs to subject to genetic tests with a better chance of finding a common gene, genes, SNiPs or deletions.
If dog owners and breeders refer diagnostic x-rays of specific pathological disorders such as Perthes Disease, coupled with pedigree information to the Pupscan study group some genetic traits may emerge.
In human research, blood clotting Factor V Leiden has been correlated with avascular necrosis and Perthes disease, but this has not yet been confirmed in dogs (Analysis of blood clotting factor activities in canine Legg-Calve-Perthes Disease. Brenig B, Leeb T., Jansen S.,Kopp T. J. Vet Intern Med Nov-Dec 1999;13(6):570-573). Sickle Cell disease is well known in humans to be a cause of avascular necrosis in bone (including Perthes Disease) and is genetically determined and perhaps similar haematological factors will be identified in dogs in time, but in 1999 none were identified.
SUFE of both hips in two dogs with no history of trauma (Bilateral epiphysiolysis of the femoral heads in two dogs. Dupuis J., Breton L., Drolet R., J Am Vet Med Assoc. 1997 Apr 15;210(8):1162-1165) would suggest an inherited condition but this appears to be rare. Hopefully if another case is identified the Veterinarian will submit samples for testing in case a genetic link can be found.
The quest for genetic causes must be applied to scanned abnormal hips between birth and eight weeks. If found, both the bitch and all the puppies should be tested. If dysplasia develops during growth without trauma or environmental (including nutritional) causes, a genome review should be arranged with the results collected on an international database.
An exciting future is in prospect!
Bibliography and References
1) Ultrasound evaluation of the Coxofemoral joints of the Canine neonate. Greshake R.J. BS, DVM, Ackerman N. DVM Veterinary Radiology & Ultrasound Vol 34 No 2 1993 pp99-104.
2) Ultrasonic and radiographic study of laxity in hip joints of young dogs. Rocha B.D., Torres R.C.S.,2007 Arq. Braz. med. Vet. Zootec, Vol 59, n1, p 90-96
3) Hereditary acetabular dysplasia in German Shepherd dogs. Henricson B. Olsson S-E J.Am.Vet.Med.Ass. 1959 135, 207
4) On the aetiology and Pathogenesis of Hip Dysplasia: a comparative review. Henricson B., Norberg I., Olsson S-E. J. Small anim.Pract. 1966 Vol 7. Pp673-688
5) Acetabular dysplasia and osteoarthritis developed by an eversion of the Acetabular Labrum.Young-Hoo Kim. 1985 Clinical Orthopaedics and Related Research 215 Feb 289-295
6) The experimental induction of subclinical Perthes Disease in the puppy following arthrotomy and intracapsular tamponade. Singleton W.B., Jones E.L. Pathology 1979 Vol 89(1) 57-71
7) Racial and geographic factors in the incidence of Legg-Calve-Perthes disease: a systematic review. Perry D.C., Machin D.M.G., Pope D., Bruce C.E., Dangerfield P., Platt M.J.., Hall A.J. Am J Epidemiol. 2012 Feb 1; 175(3):159-166
8) The Epidemiology and demographics of Legg-Calve-Perthes disease. Loder R.T., Skopelia E.N. ISRN Orthop 2011 Sep5. Doi: 10.5402/2011/504393.
9) Perthes Disease and the search for genetic associations; collagen mutations, Gaucher’s disease and Thrombophilia. Kenet G., Ezra E., Weintrob S., Steinberg D.M., Rosenberg N., Hayek S. J Bone and Joint Surg Br. 2008 Nov; 90(11): 1507-11.
10) The most severe forms of Perthes disease associated with the homozygous Factor V Leiden mutation. Szepesi K., Posan E., Harsfalvi J., et al J Bone and Joint Surg Br 2004 Apr; 86(3):426-9.
11) Analysis of blood-clotting factor activities in canine Legg-Calve-Perthes disease. Brenig B., Leeb T., Jansen S., Kopp T. J Vet Intern Med. Nov-Dec 1999:13(6):570.
12) Avascular necrosis of the Femoral Head in dogs - Retrospective study Cardoso C.B., Raral S. C., Mamprim M.J., Oliveira H. S., et al Acta Scientiae Veterinariae 2018. 46: 1537
13) Chronology of Hip Dysplasia development in a cohort of 48 Labrador Retrievers followed for Life Smith G.K., Lawler D.F., Veterinary Surgery Vol 41(1) 2012 Special Issue: advances in Hip Dysplasia. 20-33
14) Radiographic Hip Joint Phenotype of the Pembroke Welsh Corgi. Karbe G.T., Biery D.N., et al. Veterinary Surgery Vol 41 (1) Special Issue: Advances in Hip Dysplasia 34-41
15) Static and Dynamic ultrasonography for the early diagnosis of canine hip dysplasia. Fischer A., Flock A., Tellhelm B., Failing K., Kramer M., Thiel C. Journal of Small Animal Practice (2010) 51: 582-588
16) Early onset osteoarthritis in Ehlers Danlos Syndrome type VIII. Reinstein E>, Pariani M., Lachman R.S., Nemec S., Rimoin D. L., Am J Med Genet A. 2012 Apr:158A(4):938-941
17) Orthopaedic Foundation for Animals Instructions for Taking Images for OFA Dysplasia evaluations. 2021
18) The relation between Canine Hip Dysplasia, Genetic Diversity and Inbreeding by Breed. Comhaire F. Open Journal of Veterinary Medicine Vol 4 No 5(2014) Article ID:45804
19) A Post Mortem Study of the hip joint. Byers P.D., Contepomi C.A., Farkas T.A. Ann Rheum Dis.1970 Vol 29:15-31.
20) Intra-articular acetabular labrum; a possible aetiological factor in certain cases of osteoarthritis of the hip. Harris W.H., Bourne R.B, Oh I., J Bone and Joint Surg. 1979 Vol 61A: 510-514
21) The torn acetabular labrum. Dorrell J.H., Catterall A. J Bone and joint Surg 1986 Vol 68B: 400-403
22) Labral lesions; an elusive source of hip pain. Byrd J.W. Arthroscopy 1996 Vol 12:603-612
23) Development of the acetabular roof in the fetal hip. Laurenson R.D., J Bone and joint Surgery 1965.Vol47A: 975-983.
24) Growth and Development of the acetabulum in the normal child. Ponseti I.V. J Bone and Joint Surgery 1978 Vol 60A;575-585.
25) Anatomy, Histologic features and Vascularity of the adult acetabular labrum. Seldes R.M.,Tan V., Hunt J., Katz., Winiarsky R., Fitzgerald R.H.Jr Clinical Orthopaedics and Related Research 2001 Vol 382; 232-240.
26) Os acetabuli in femoro-acetabular impingement; stress fracture or unfused secondary ossification centre of the acetabular rim? Martinez A.E., Li S.M., Ganz R., Beck M. Hip Int.2006 Oct-Dec:16(4);281-286.
27) The aetiology of Primary Arthritis of the hip. Murray R.O. B J Radiology 1964 Vol 38.
28) Mode of inheritance of Perthes Disease in Manchester Terriers. Vasseur P.B.,Foley P., Stevenson S., Heitter D. Clinical Orthopaedics and Related Research July 1989 244:281-292.
29) Bilateral epiphysiolysis of the femoral heads in two dogs. Dupuis J, Breton L., Drolet R. J Am Vet Med Assoc 1997 Apr 15;210(8);1162-1165.
30) The endocrine basis for slipping of the upper femoral epiphysis. Harris W.R. Journal of Bone and Joint Surgery Vol 32(B) No 1 Feb 1950
31) Bone age in children of Diverse Ethnicity. Ontell F.K., Ivanovic M., Ablin D.S., Barlow T.W. American Journal of Roentgenology 1996;167:1395-1398.
32) Osteonecrosis of the femoral head of Laboratory Animals: the lessons learned from a comparative Study of osteonecrosis in Man and Experimental Animals. 2003 Boss J.H., Misselevich I. Vet.Pathol 40:345-354
33) Housing- and exercise-related risk factors associated with the development of hip dysplasia as determined by radiographic evaluation in a prospective cohort of Newfoundlands, Labrador Retrievers, Leonbergers and Irish Wolfhounds in Norway. Krontveit R. I., Nodtvedt A.,Saevik B., Ropstad E., Trangerud C. American Journal of Veterinary Research 2012; Vol73 No 6:838-846.
34) Seasonal variation in the hip score of dogs as assessed by the New Zealand Veterinary Association Hip Dysplasia scheme. Worth A.J., Bridges J.P., Cave N.J., Jones G. New Zealand Veterinary Journal 2012 Vol 60 No 2.
35) Prevalence, duration and risk factors for appendicular osteoarthritis in a UK dog population under primary veterinary care. Anderson K.L., O’Neill D.G., Brodbelt D.C. et al . Nature Scientific Reports (2018)8:5641
36) The relation between canine hip dysplasia, Genetic Diversity and In-Breeding by Breed. Comhaire F.H. Open Journal of Veterinary Medicine Vol4 No.5(2014) Article ID;45804.
37) Confirmation that a deletion in the POMC gene is associated with body weight in Labrador Retriever dogs. Mankowska M. Krzeminska P. Graczyk M. Switonski M., Res. Vet. Sci 2017 Jun;112:116-118.
38) Personal communication pending publication.
39) Intracapsular and Atmospheric pressure in the dynamics and stability of the hip. Wingstrand H. Wingstrand A. Kranz P., Acta Orthopaedica Scandinavica 1990;61(3): 231-235.